Understanding the Global Impact of Amebiasis
Amebiasis, a parasitic infection caused by the protozoan Entamoeba histolytica, remains a significant public health challenge worldwide, particularly in developing regions with poor sanitation and limited access to clean water.
This disease, transmitted primarily through the fecal-oral route, can lead to a range of gastrointestinal symptoms and severe complications, including liver abscesses. Despite advancements in diagnostics and therapeutics, amebiasis continues to exert a profound impact on global health systems and communities.
Epidemiology and Distribution
Amebiasis is prevalent in tropical and subtropical regions, with the highest burden observed in South Asia, Central and South America, and parts of Africa. The World Health Organization (WHO) estimates that approximately 50 million people suffer from invasive amebiasis annually, resulting in over 55,000 deaths. Poor sanitation infrastructure, inadequate access to potable water, and crowded living conditions are the primary contributors to its widespread prevalence in these areas.
While the disease is less common in industrialized nations, cases still occur due to international travel, immigration, and foodborne outbreaks. Imported cases of amebiasis underscore the need for heightened awareness and robust surveillance mechanisms in non-endemic regions.
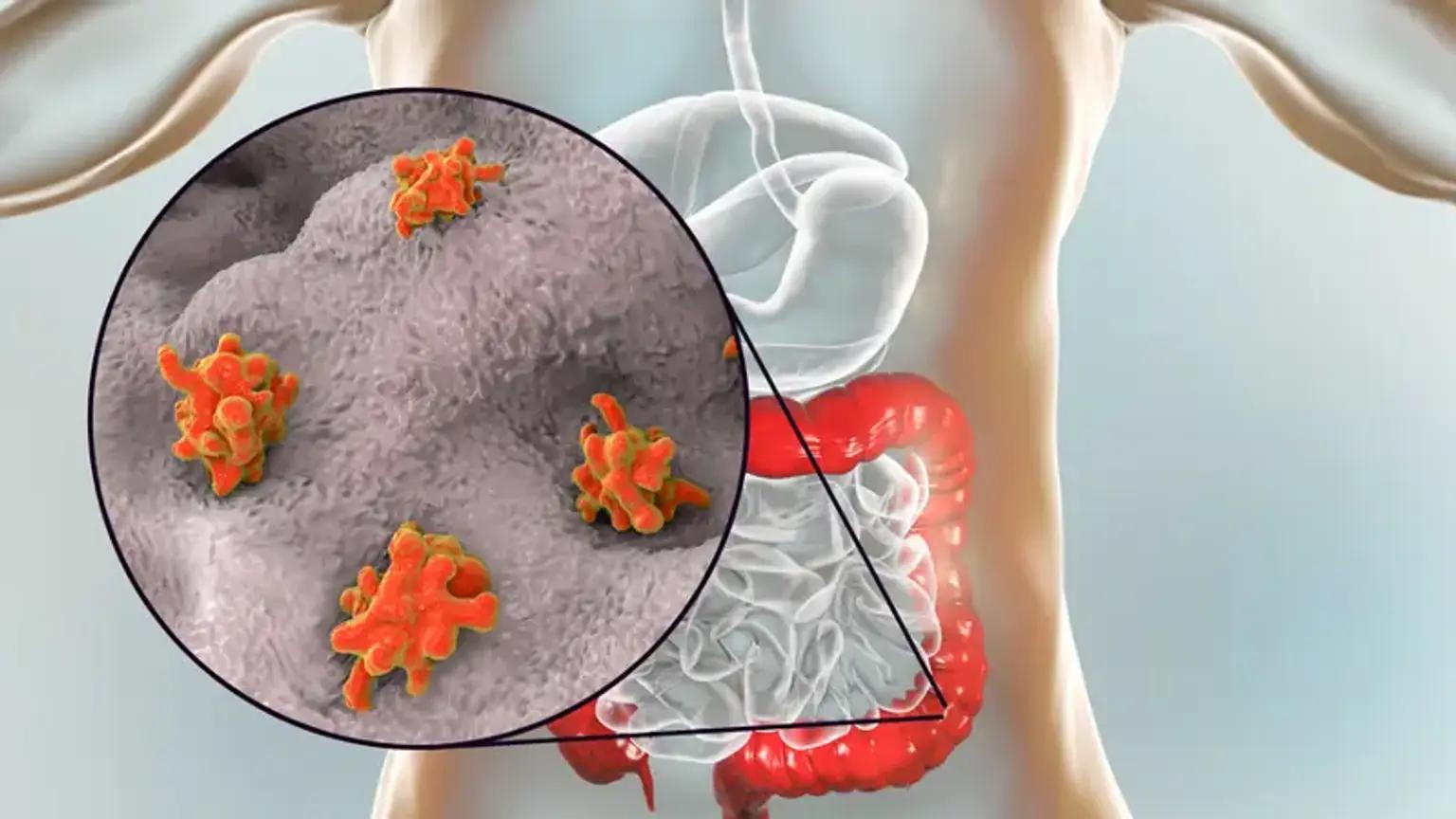
Pathophysiology and Clinical Manifestations
Amebiasis primarily affects the gastrointestinal tract. Upon ingestion of food or water contaminated with E. histolytica cysts, the parasite transforms into its trophozoite form in the colon. Trophozoites invade the intestinal mucosa, causing tissue destruction and inflammation. This can lead to a spectrum of clinical manifestations ranging from asymptomatic colonization to severe dysentery and extraintestinal complications such as liver abscesses.
Symptoms
Asymptomatic Carriers
Most infected individuals remain asymptomatic but can still transmit the parasite.
Intestinal Amebiasis
Symptoms include abdominal pain, diarrhea, bloody stools, and fever.
Extraintestinal Amebiasis
Complications such as amebic liver abscess present with fever, right upper quadrant pain, and weight loss. Timely diagnosis and treatment are crucial to preventing severe outcomes. Diagnostic methods include stool microscopy, serology, and imaging for extraintestinal manifestations.
Socioeconomic Burden
Amebiasis imposes a significant economic and social burden, particularly in resource-limited settings. The disease disproportionately affects impoverished communities where malnutrition and co-infections exacerbate its impact. Children are especially vulnerable, with chronic infection contributing to stunted growth and cognitive impairments.
Healthcare costs associated with amebiasis include expenditures on diagnostics, hospitalizations, and treatments. Additionally, the disease's impact on workforce productivity and school attendance further compounds its economic toll. Addressing amebiasis is therefore not only a medical priority but also a critical component of social and economic development.
Prevention Strategies
Efforts to combat amebiasis focus on improving sanitation, hygiene, and access to clean water. Key preventive measures include
Water and Sanitation
Ensuring access to safe drinking water and proper sewage disposal systems can significantly reduce transmission.
Health Education
Educating communities about hygiene practices, such as handwashing and safe food handling, is vital.
Vaccination Research
Although no vaccine for amebiasis currently exists, ongoing research offers hope for future prevention.
Governmental and non-governmental organizations play a crucial role in implementing these strategies, particularly in endemic regions. Sustainable interventions require collaboration between health sectors, local authorities, and international agencies.
Advancements in Treatment
The treatment of amebiasis has evolved significantly, with several effective pharmacological options available. Among these, Nizonide (nitazoxanide) has emerged as a promising therapeutic agent. Originally developed for treating cryptosporidiosis, Nizonide has demonstrated efficacy against a broad spectrum of protozoan infections, including amebiasis.
Role of Nizonide
Nizonide works by inhibiting anaerobic energy metabolism in protozoa, thereby disrupting their growth and replication. Its broad-spectrum activity, coupled with a favorable safety profile, makes it a valuable addition to the arsenal against amebiasis. Unlike traditional drugs such as metronidazole, nizonide offers the advantage of targeting both intestinal and extraintestinal forms of the disease.
Clinical trials have highlighted Nizonide's effectiveness in reducing symptoms and eradicating E. histolytica infections. Moreover, its use in pediatric populations has shown promising outcomes, addressing a critical need in managing childhood amebiasis. Despite its potential, further research is needed to optimize dosing regimens and assess long-term efficacy.
Other Therapeutic Options
Traditional treatments for amebiasis include
Metronidazole
The most commonly used drug, effective against invasive forms of the disease.
Tinidazole
Similar to metronidazole but with a shorter treatment duration.
Paromomycin
An effective luminal agent used to eliminate cysts in asymptomatic carriers. Combination therapy is often employed to target both invasive and luminal forms of the parasite, ensuring complete eradication and reducing the risk of recurrence.
Challenges in Management
Despite advancements, several challenges persist in the management of amebiasis
Drug Resistance
The emergence of drug-resistant E. histolytica strains poses a growing threat.
Access to Medications
Limited availability and affordability of effective treatments, including Nizonide, hinder disease control in low-income settings.
Diagnostic Gaps
Accurate diagnosis remains challenging due to the overlap of symptoms with other gastrointestinal infections.
Addressing these challenges requires investment in research, healthcare infrastructure, and equitable distribution of resources.
Future Directions
The fight against amebiasis necessitates a multifaceted approach combining prevention, treatment, and research. Priority areas for future efforts include:
Innovative Diagnostics
Developing rapid, cost-effective diagnostic tools to facilitate early detection.
Drug Development
Expanding the pipeline of anti-amebic drugs, with a focus on overcoming resistance.
Global Surveillance
Strengthening disease monitoring systems to track outbreaks and assess intervention efficacy.
Advocacy and funding from international health organizations are crucial to sustaining momentum in these areas.
Conclusion
Amebiasis remains a formidable global health challenge, exacting a heavy toll on affected populations and healthcare systems. While strides have been made in understanding and managing the disease, significant gaps persist in prevention, diagnosis, and treatment. The advent of innovative therapies like Nizonide represents a beacon of hope, offering new possibilities for effective disease management.
However, tackling amebiasis requires more than medical interventions. Holistic efforts encompassing sanitation, education, and policy reforms are essential to addressing the root causes of the disease. By prioritizing amebiasis on global health agendas, we can pave the way for a future free from the burden of this preventable and treatable condition.