The Role of ELISA and Immunofluorescence in Assessing Long-Term Antibody Responses
Though the COVID-19 pandemic may have somewhat faded from the forefront of public attention, its enduring impact persists. Nations worldwide have grappled with recurring waves of infection over the past three years, despite many establishing immunity barriers. However, concerns about long COVID symptoms and the potential for recurrent infections persist, posing significant challenges to individuals' immune systems.
In a year-long follow-up study, a research team investigated the antibody response of COVID-19 patients, exploring the relationship between antibody response and neutralizing antibody activity. Recently published in the Frontiers in Immunology journal under the title "Evaluation of Humoral Immune Response in Relation to COVID-19 Severity Over 1 Year Post-Infection: Critical Cases Show a Higher Humoral Immune Response Than Mild Cases," this study sheds light on the enduring dynamics of SARS-CoV-2-specific B cell memory among recovered COVID-19 patients.
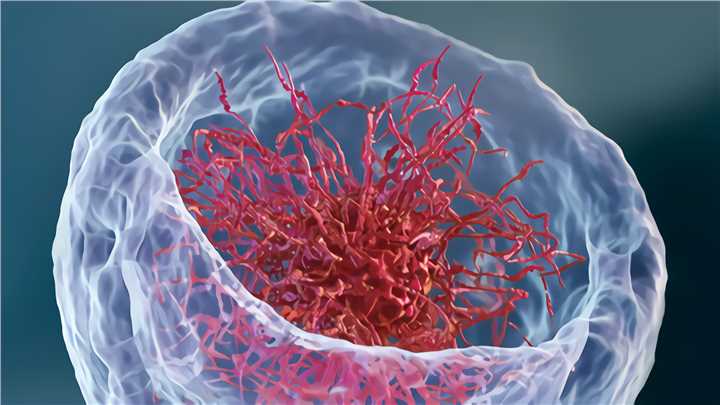
Monitoring antibody levels in individuals who have recovered from COVID-19 or have been vaccinated remains paramount. The research team employed various methods to accomplish this task, including utilizing the recombinant protein of the SARS-CoV-2 spike S1 domain as an antigen and employing the indirect enzyme-linked immunosorbent assay (ELISA) to detect IgG antibodies in COVID-19 patients.
ELISA, a plate-based assay technique, facilitates the detection and quantification of peptides, proteins, and hormones. It relies on specific antigen-antibody binding and utilizes enzymes. In this process, an antigen (or antibody) is immobilized on a solid surface, followed by the addition of enzyme-conjugated antibodies after incubation with specific antibodies (or antigens). Detection involves evaluating conjugated enzyme activity through incubation with a substrate to yield a quantifiable result.
The team also utilized indirect immunofluorescence (IIF) by infecting Vero E6 cells with SARS-CoV-2 samples obtained from the Korea Centers for Disease Control and Prevention. IIF is a two-step serological technique used to identify circulating autoantibodies in a patient's serum. This method involves a primary, unlabeled antibody binding to the target, followed by a fluorophore-labeled secondary antibody to detect the primary antibody. Although more complex and time-consuming, IIF is more sensitive due to the ability of more than one secondary antibody to bind to each primary antibody, thus amplifying the fluorescence signal.
By observing the distribution and localization of specific antibodies within cells and tissues, IIF provides valuable insights into the effectiveness of the immune response. Using ELISA and IF in tandem aids in the development of targeted and personalized treatment strategies for post-COVID care.
In the quest for more effective COVID-19 management, human anti-SARS-CoV-2 spike recombinant antibody (CR3022 antibody) therapy emerges as a promising avenue. By targeting the spike protein of the virus, CR3022 can neutralize SARS-CoV-2 and potentially inhibit viral infection. Incorporating CR3022 antibody therapy into post-COVID care, alongside the monitoring provided by ELISA and IF, may offer enhanced protection, particularly for high-risk individuals and those with compromised immune systems.
In addition to the CR3022 antibody, other anti-SARS-CoV-2 RBD antibodies, such as mouse anti-SARS-CoV-2 recombinant antibody, have also been developed against the novel coronavirus. Alongside antibody-focused strategies, maintaining essential public health measures such as mask-wearing, social distancing, and vaccination remains critical to curbing the virus's spread and preventing new variants.